Beta adrenergic Blockers
Beta adrenergic Blockers
Betaadrenergic blockers are antianginals, an tiarrhythmics, and antihypertensives. These drugs competitively block betaadrenergic re ceptors in the heart and juxtaglomerular apparatus. They decrease the influence of the sympathetic nervous system on these tissues, the excitability of the heart, cardiac workload, oxy gen consumption, and the release of renin; they lower BP. They have membranestabilizing (lo cal anesthetic) effects that contribute to their antiarrhythmic action. They also act in the CNS to reduce sympathetic outflow and vasocon strictor tone.
Indications
Hypertension (alone or with other drugs, es pecially diuretics) Angina pectoris caused by coronary ather osclerosis Hypertrophic subaortic stenosis, to manage associated stressinduced angina, palpita tions, and syncope; cardiac arrhythmias, es pecially supraventricular tachycardia, and ventricular tachycardias induced by digox in or catecholamines; essential tremor, fa milial or hereditary Prevention of reinfarction in clinically sta ble patients when started 1–4 wk after MI Adjunctive therapy for pheochromocytoma after treatment with an alphaadrenergic blocker, to manage tachycardia before or during surgery or if the pheochromocytoma is inoperable Prophylaxis for migraine headache (pro pranolol) Management of acute situational stress re action (stage fright); essential tremor (pro pranolol) Unlabeled uses: Treatment of recurrent GI bleeding in cirrhotic patients, schizophrenia, tardive dyskinesia, acute panic symptoms, vaginal contraceptive, acute alcohol with drawal Contraindications and cautions
Contraindicated with allergy to beta adrenergic blockers, sinus bradycardia, second or thirddegree heart block, cardio genic shock, heart failure, bronchial asthma, bronchospasm, COPD, pregnancy (neonatal bradycardia, hypoglycemia, and apnea have occurred in infants whose mothers received propranolol; low birth weight occurs with chronic maternal use during pregnancy), or lactation. Use cautiously with hypoglycemia and dia betes, thyrotoxicosis, hepatic impairment. Adverse effects
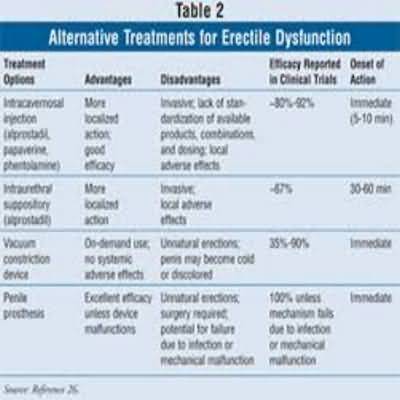
Allergic reactions: Pharyngitis, erythe matous rash, fever, sore throat, laryngo spasm, respiratory distress CV: Bradycardia, heart failure, cardiac arrhythmias, sinoatrial or AV nodal block, tachycardia, peripheral vascular insuffi ciency, claudication, stroke, pulmonary edema, hypotension Dermatologic: Rash, pruritus, sweating, dry skin EENT: Eye irritation, dry eyes, conjunctivi tis, blurred vision GI: Gastric pain, flatulence, constipation, diarrhea, nausea, vomiting, anorexia, ischemic colitis, renal and mesenteric Betaadrenergic Blockers arterialthrombosis, retroperitoneal fibrosis, hepatomegaly, acute pancreatitis GU: Impotence, decreased libido,Peyronie’s disease, dysuria, nocturia, frequency Musculoskeletal: Joint pain, arthralgia, muscle cramps Neurologic: Dizziness, vertigo, tinnitus, fatigue,emotional depression, paresthesias, sleep disturbances, hallucinations, disori entation, memory loss, slurred speech Respiratory: Bronchospasm, dyspnea, cough, bronchial obstruction, nasal stuffi ness, rhinitis, pharyngitis Other: Decreased exercise tolerance, de velopment of antinuclear antibodies, hyperglycemia or hypoglycemia, elevated serum transaminase, alkaline phosphatase, and LDH Interactions
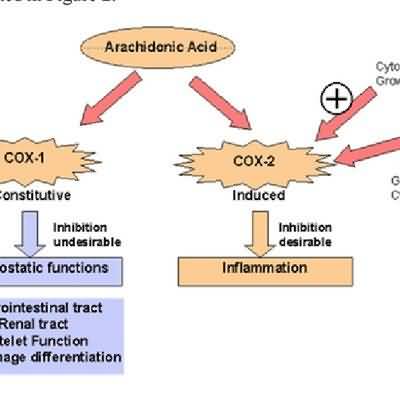
Drugdrug Increased effects with ver apamil, diltiazem Decreased effects with in domethacin, ibuprofen, piroxicam, sulindac, barbiturates Prolonged hypoglycemic effects of insulin with betaadrenergic blockers Pe ripheral ischemia possible if combined with ergot alkaloids Initial hypertensive episode followed by bradycardia with epinephrine In creased “firstdose response” to prazosin with betaadrenergic blockers Increased serum lev els and toxic effects with lidocaine, cimetidine Increased serum levels of betaadrenergic blockers and phenothiazines, hydralazine if the two drugs are taken concurrently Paradoxi cal hypertension when clonidine is given with betaadrenergic blockers; increased rebound hypertension when clonidine is discontinued Decreased serum levels and therapeutic effects if taken with methimazole, propylthiouracil Decreased bronchodilator effects of theo phyllines Decreased antihypertensive effects with NSAIDs (eg, ibuprofen, indomethacin, piroxicam, sulindac), rifampin ?Druglab test Interference with glucose or insulin tolerance tests, glaucoma screening tests Nursing considerations
Assessment
History: Allergy to betaadrenergic block ers, sinus bradycardia, second or third degree heart block, cardiogenic shock, heart failure, bronchial asthma, bronchospasm, COPD, hypoglycemia and diabetes, thyro toxicosis, hepatic impairment, pregnancy, lactation Physical: Weight, skin color, lesions, edema, T; reflexes, affect, vision, hearing, orientation; BP, P, ECG, peripheral perfusion; R, auscul tation; bowel sounds, normal output, liver evaluation; bladder palpation; LFTs, thyroid function test, blood and urine glucose Interventions
Do not stop drug abruptly after longterm therapy (hypersensitivity to catecholamines may have developed, causing exacerbation of angina, MI, and ventricular arrhythmias). Taper drug gradually over 2 wk with moni toring. Consult physician about withdrawing drug if patient is to undergo surgery (contro versial). Give oral drug with food to facilitate ab sorption. Provide side rails and assistance with walk ing if CNS, vision changes occur. Position patient to decrease effects of ede ma, respiratory obstruction. Space activities, and provide rest periods. Provide frequent small meals if GI effects occur. Provide comfort measures to help patient cope with eye, GI, joint, CNS, dermatologic effects. Teaching points
Take these drugs with meals. Do not stop taking these drugs abruptly; this can wors en the disorder being treated. If you have diabetes, the normal signs of hypoglycemia (tremor, tachycardia) may be blocked by these drugs; monitor your blood or urine glucose carefully; be sure to eat reg ular meals, and take your diabetic medica tion regularly. You may experience these side effects: Dizzi ness, drowsiness, lightheadedness, blurred vision (avoid driving or performing haz ardous tasks); nausea, loss of appetite (fre quent small meals may help); nightmares, depression (notify your health care provider, who may be able to change your medication); sexual impotence (you may want to discuss this with your health care provider). Adverse effects
in italics are most common; those in bold are lifethreatening. U Do not crush. 36 ? Beta adrenergic Blockers (?-blockers) Report difficulty breathing, night cough, swelling of extremities, slow pulse, confu sion, depression, rash, fever, sore throat. Representative drugs
acebutolol atenolol betaxolol bisoprolol carvedilol esmolol labetalol levobunolol metipranolol metoprolol nadolol nebivolol penbutolol pindolol propranolol sotalol timolol