Antiarrhythmics
Antiarrhythmics
Antiarrhythmics act at specific sites to alter the action potential of cardiac cells and in- terfere with the electrical excitability of the heart. Most of these drugs may cause new or worsened arrhythmias (proarrhythmic ef- fect) and must be used with caution and with continual cardiac monitoring and patient evaluation.
Indications
Treatment of tachycardia when rapid but short-term control of ventricular rate is de- sirable (patients with atrial fibrillation, atrial flutter, in both perioperative and post- operative situations) Treatment of noncompensatory tachycar- dia when heart rate requires specific inter- vention Treatment of atrial arrhythmias Contraindications and cautions
There are no Contraindications
; reserve for emergency situations. Use cautiously during pregnancy or lactation. Adverse effects
CNS: Light-headedness, speech disorder, midscapular pain, weakness, rigors,som- nolence, confusion CV: Hypotension,pallor, arrhythmias GI: Taste perversion GU: Urine retention Local: Inflammation, induration, ede- ma, erythema, burning at the site of infusion Other: Fever, rhonchi, flushing Interactions
Drug-drug Increased risk of drug inter- actions with antiarrhythmic use; monitor pa- tients Nursing considerations
Assessment
History: Cardiac disease, cerebrovascular disease Physical: P, BP, ECG; orientation, reflex- es; R, adventitious sounds; urinary output Interventions
Ensure that more toxic drug is not used in chronic settings when transfer to another drug is anticipated. Monitor BP, heart rate, and rhythm closely. Provide comfort measures for pain, rigors, fever, flushing, if patient is awake. Provide supportive measures appropriate to condition being treated. Provide support and encouragement to deal with drug effects and discomfort of IV lines. Monitor drug levels for procainamide and amiodarone, as indicated. Teaching points
Reserved for emergency use. Incorporate in- formation about these drugs into the over- all teaching program for patient. Patients maintained on oral drugs will need specif- ic teaching. Representative drugs
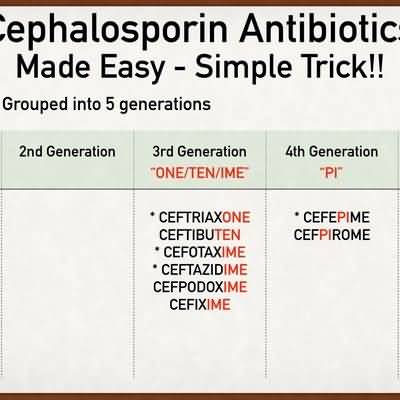
Type IA disopyramide quinidine Type IB lidocaine mexiletine phenytoin Type IC flecainide propafenone Type II acebutolol esmolol propranolol Type III amiodarone dofetilide ibutilide sotalol Type IV diltiazem verapamil Other adenosine digoxin dronedarone