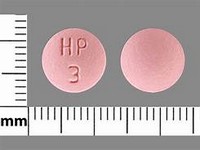
indometacin

indometacin
CLINICAL USE
NSAID:Pain and inflammation in rheumatic disease and other musculoskeletal disordersAcute gout Dysmenorrhoea Closure of ductus arteriosus
DOSE IN NORMAL RENAL FUNCTION
Oral: 50–200 mg daily in divided doses, after foodPR: 100 mg twice daily if required Gout: 150–200 mg daily in divided doses Dysmenorrhoea: up to 75 mg daily Maximum combined oral and PR: 150– 200 mg daily
PHARMACOKINETICS
Molecular weight :357.8 %Protein binding :90–99 %Excreted unchanged in urine : 5–20 (60% as metabolites) Volume of distribution (L/kg) :0.34–1.57half-life – normal/ESRD (hrs) :1–16/unchanged DOSE IN RENAL IMPAIRMENT
GFR (mL/MIN)
20 to 50 : Dose as in normal renal function, but avoid if possible 10 to 20 : Dose as in normal renal function, but avoid if possible <10 : Dose as in normal renal function, but only use if CKD 5 and on dialysis DOSE IN PATIENTS UNDERGOING RENAL REPLACEMENT THERAPIES
CAPD :Not dialysed. Dose as in normal renal function HD :Not dialysed. Dose as in normal renal function HDF/high flux :Unlikely to be dialysed. Dose as in normal renal function CAV/VVHD :Not dialysed. Dose as in GFR=10–20 mL/min IMPORTANT DRUG INTERACTIONS
Potentially hazardous interactions with other drugsACE inhibitors and angiotensin-II antagonists: antagonism of hypotensive effect; increased risk of nephrotoxicity and hyperkalaemiaAnalgesics: avoid concomitant use of 2 or more NSAIDs, including aspirin (increased side effects); avoid with ketorolac (increased risk of side effects and haemorrhage)Antibacterials: possibly increased risk of convulsions with quinolonesAnticoagulants: effects of coumarins and phenindione enhanced; possibly increased risk of bleeding with heparinsAntidepressants: increased risk of bleeding with SSRIs and venlafaxineAntidiabetic agents: effects of sulphonylureas enhancedAnti-epileptic agents: effects of phenytoin enhancedAntipsychotics: possible severe drowsiness with haloperidolAntivirals: increased risk of haematological toxicity with zidovudine; concentration possibly increased by ritonavirCiclosporin: increased risk of nephrotoxicityCytotoxic agents: reduced excretion of methotrexate Diuretics: increased risk of nephrotoxicity, hyperkalaemia with potassium-sparing diuretics; antagonism of diuretic effect Lithium: lithium excretion reduced Pentoxifylline: possibly increased risk of bleedingProbenecid: excretion of indometacin reduced Tacrolimus: increased risk of nephrotoxicity ADMINISTRATION
Reconstition
– Route
Oral, PR, IV Rate of Administration
20–30 minutes Comments
–.382 indoMETACin OTHER INFORMATION
Inhibition of renal prostaglandin synthesis by NSAIDs may interfere with renal function, especially in the presence of existing renal disease – avoid if possible; if not, check serum creatinine 48–72 hours after starting NSAID – if raised, discontinue NSAID therapyUse normal doses in patients with ERF on dialysis if they do not pass any urineUse with caution in renal transplant recipients – can reduce intrarenal autocoid synthesis.
See how to identify renal failure stages according to GFR calculation
See how to diagnose irreversible renal disease
Home