snoring
snoring
ESSENTIALS OF DIAGNOSIS
General Considerations
Ventilation disorders during sleep are extremely commonWhile OSA occurs in 5–10% of Americans, clinically relevant snoring may occur in as many as 59%
In general, sleep-disordered breathing problems are attributed to narrowing of the upper aerodigestive tract during sleep due to changes in position, muscle tone, and soft tissue hypertrophy or laxity
The most common sites of obstruction are the oropharynx and the base of the tongue
The spectrum of the problem ranges from simple snoring without cessation of airflow to OSA with long periods of apnea and lifethreatening physiologic sequelae
OSA is discussed in Chapter 9
In contrast to OSA, snoring is almost exclusively a social problem, and despite its prevalence and association with OSA, there is comparatively little known about the management of this problem
Clinical Findings
All patients who complain of snoring should be evaluated for OSA as discussed in Chapter 9
Symptoms of OSA (including snoring, excessive daytime somnolence, daytime headaches, and weight gain) may be present in as many as 30% of patients without demonstrable apnea or hypopnea on formal testing
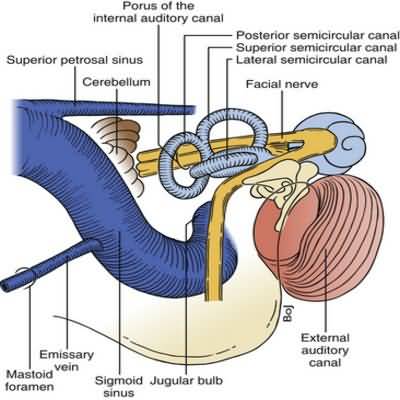
Clinical examination should include examination of the nasal cavity, nasopharynx, oropharynx, and larynx to help exclude other causes of dynamic airway obstruction
In many cases of isolated snoring, the palate and uvula appear enlarged and elongated with excessive mucosa hanging below the muscular portion of the soft palate
Sleep examination with polysomnography is strongly advised in the evaluation of a patient with complaints of snoring
Radiographic imaging of the head or neck is generally not necessary
Treatment
Expeditious and inexpensive management solutions of snoring are sought, often with little or no benefitDiet modification and physical exercise can lead to improvement in snoring through the weight loss and improvement in pharyngeal tone that accompanies overall physical conditioning
Position change during sleep can be effective, and time-honored treatments, such as taping or sewing a tennis ball to the back of a shirt worn during sleep, may satisfactorily eliminate symptoms by ensuring recumbency on one side
Although numerous pharmacologic therapies have been endorsed, none demonstrate any significant utility when scrutinized
Anatomic management of snoring can be challenging
As with OSA, snoring can come from a number of sites in the upper aerodigestive tract
While medical or surgical correction of nasal obstruction may help alleviate snoring problems, most interventions aim to improve airflow through the nasopharynx and oropharynx
Nonsurgical options include mandibular advancement appliances designed to pull the base of the tongue forward and continuous positive airway pressure via face or nasal mask
Compliance with both of these treatment options is problematic because snorers without OSA do not notice the physiologic benefits of these devices noted by patients with sleep apnea
Surgical correction of snoring is most commonly directed at the soft palate
Historical approaches involved resection of redundant mucosa and the uvula similar to uvulopalatopharyngoplasty that is used for OSA
Regardless of how limited the procedure or what technique was used, postoperative pain, the expense of general anesthesia, and high recurrence rates limit the utility of these procedures
Office-based approaches are more widely used because of these limitations
Most of these procedures aim to stiffen the palate to prevent vibration rather than remove it
A series of procedures, including injection snoreplasty, radiofrequency thermal fibrosis, and an implantable palatal device, have been used with variable success and patient tolerance
The techniques can be technically challenging
Persistent symptoms may occur following initial treatment necessitating costly (and sometimes painful) repeat procedures
The durability of these procedures in alleviating symptoms is also poorly understood, and late failures can lead to patient and clinician frustration