leukoplakia
leukoplakia
ESSENTIALS OF DIAGNOSIS
Ulceration may be present
Leukoplakic regions range from small to several centimeters in diameter
Histologically, they are often hyperkeratoses occurring in response to chronic irritation (eg, from dentures, tobacco, lichen planus); about 2–6%, however, represent either dysplasia or early invasive squamous cell carcinoma
Distinguishing between leukoplakia and erythroplakia is important because about 90% of cases of erythroplakia are either dysplasia or carcinoma
Squamous cell carcinoma accounts for 90% of oral cancer
Alcohol and tobacco use are the major epidemiologic risk factors
The differential diagnosis may include oral candidiasis, necrotizing sialometaplasia, pseudoepitheliomatous hyperplasia, median rhomboid glossitis, and vesiculoerosive inflammatory disease, such as erosive lichen planus
This should not be confused with the brown-black gingival melanin pigmentation—diffuse or speckled—common in nonwhites, blue-black embedded fragments of dental amalgam, or other systemic disorders associated with general pigmentation (neurofibromatosis, familial polyposis, Addison disease)
Intraoral melanoma is extremely rare and carries a dismal prognosis
Any area of erythroplakia, enlarging area of leukoplakia, or a lesion that has submucosal depth on palpation should have an incisional biopsy or an exfoliative cytologic examination
Ulcerative lesions are particularly suspicious and worrisome
Specialty referral should be sought early both for diagnosis and treatment
A systematic intraoral examination—including the lateral tongue, floor of the mouth, gingiva, buccal area, palate, and tonsillar fossae—and palpation of the neck for enlarged lymph nodes should be part of any general physical examination, especially in patients over the age of 45 who smoke tobacco or drink immoderately
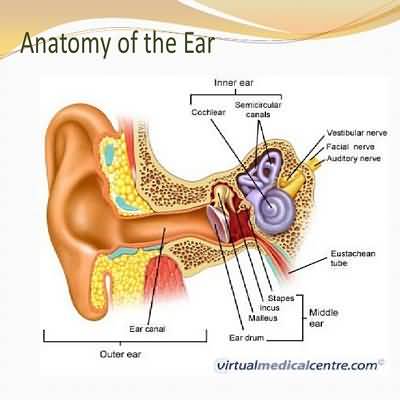
Indirect or fiberoptic examination of the nasopharynx, oropharynx, hypopharynx, and larynx by an otolaryngologist, head and neck surgeon, or radiation oncologist should also be considered for such patients when there is unexplained or persistent throat or ear pain, oral or nasal bleeding, or oral erythroplakia
Fine-needle aspiration (FNA) biopsy may expedite the diagnosis if an enlarged lymph node is found
To date, there remain no approved therapies for reversing or stabilizing leukoplakia or erythroplakia
Clinical trials have suggested a role for beta-carotene, celecoxib, vitamin E, and retinoids in producing regression of leukoplakia and reducing the incidence of recurrent squamous cell carcinomas
None have demonstrated benefit in large studies and these agents are not in general use today
The mainstays of management are surveillance following elimination of carcinogenic irritants (eg, smoking tobacco, chewing tobacco or betel nut, drinking alcohol) along with serial biopsies and excisions
Oral lichen planus is a relatively common (0
5–2% of the population) chronic inflammatory autoimmune disease that may be difficult to diagnose clinically because of its numerous distinct phenotypic subtypes
For example, the reticular pattern may mimic candidiasis or hyperkeratosis, while the erosive pattern may mimic squamous cell carcinoma
Management begins with dis- tinguishing it from other oral lesions
Exfoliative cytology or a small incisional or excisional biopsy is indicated, especially if squamous cell carcinoma is suspected
Therapy of lichen planus is aimed at managing pain and discomfort
Corticosteroids have been used widely both locally and systemically
Cyclosporines and retinoids have also been used, but tacrolimus shows the most promise in recent studies
Many experts think there is a low rate (1%) of squamous cell carcinoma arising within lichen planus (in addition to the possibility of clinical misdiagnosis)
Hairy leukoplakia occurs on the lateral border of the tongue and is a common early finding in HIV infection (see Chapter 31)
It often develops quickly and appears as slightly raised leukoplakic areas with a corrugated or “hairy” surface (Figure 8–6)
While much more prevalent in HIV-positive patients, hairy leukoplakia can occur following solid organ transplantation and is associated with Epstein-Barr virus infection and long-term systemic corticosteroid use
Hairy leukoplakia waxes and wanes over time with generally modest irritative symptoms
Acyclovir, valacyclovir, and famciclovir have all been used for treatment but produce only temporary resolution of the condition
It does not appear to predispose to malignant transformation
Oral cavity squamous cell carcinoma can be hard to distinguish from other oral lesions, but early detection is the key to successful management
Raised, firm, white lesions with ulcers at the base are highly suspicious and generally quite painful on even gentle palpation
Lesions less than 4 mm in depth have a low propensity to metastasize
Most patients in whom the tumor is detected before it is 2 cm in diameter are cured by local resection
Radiation is reserved for patients with positive margins or metastatic disease
Large tumors are usually treated with a combination of resection, neck dissection, and external beam radiation
Reconstruction, if required, is done at the time of resection and can involve the use of myocutaneous flaps or vascularized free flaps with or without bone
Oropharyngeal squamous cell carcinoma generally presents later than oral cavity squamous cell carcinoma
The lesions tend to be larger and are often buried within the lymphoid tissue of the palatine or lingual tonsils
Most patients note only unilateral odynophagia and weight loss, but ipsilateral cervical lymphadenopathy is often identified by the careful clinician
While these tumors are typically associated with known carcinogens such as tobacco and alcohol, their epidemiology has changed dramatically over the past 20 years
Despite demonstrated reductions in tobacco and alcohol use within developed nations, the incidence of oropharyngeal squamous cell carcinoma has not declined over this period
Known as a possible cause of head and neck cancer since 1983, the human papillomavi- rus (HPV)—most commonly, type 16—is now believed to be the cause of up to 70% of all oropharyngeal squamous cell carcinoma
HPV-positive tumors are readily distinguished by immunostaining of primary tumor or fineneedle aspiration biopsy specimens for the p16 protein, a tumor suppressor protein that is highly correlated with the presence of HPV
These tumors often present in advanced stages of the disease with regional cervical lymph node metastases (stages III and IV), but have a better prognosis than similarly staged lesions in tobacco and alcohol users
This difference in disease control is so apparent in multicenter studies that, based on the presence or absence of the p16 protein, two distinct staging systems for oropharyngeal squamous cell carcinoma were introduced in 2018
Ongoing clinical trials are trying to determine if a reduction in treatment intensity is warranted for HPV-associated cancers