epistaxis
epistaxis
ESSENTIALS OF DIAGNOSIS
When this is inadequate, topical sympathomimetics and various nasal tamponade methods are usually effective
General Considerations
Epistaxis is an extremely common problem in the primary care settingPredisposing factors include nasal trauma (nose picking, foreign bodies, forceful nose blowing), rhinitis, nasal mucosal drying from low humidity or supplemental nasal oxygen, deviation of the nasal septum, atherosclerotic disease, hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome), inhaled nasal cocaine or other drug use, and alcohol use
Poorly controlled hypertension has traditionally been associated with epistaxis, although confounding factors during bleeding events make establishing a causal relationship impossible
Anticoagulation or antiplatelet medications may be associated with a higher incidence of epistaxis, more frequent recurrence of epistaxis, and greater difficulty controlling bleeding, but they do not cause epistaxis
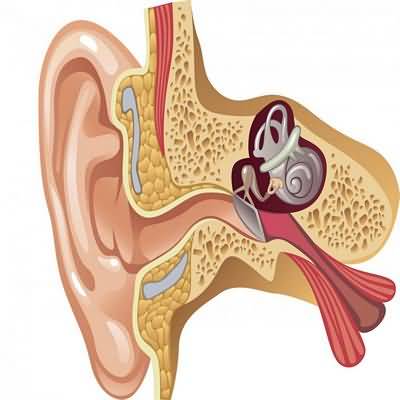
Bleeding is most common in the anterior septum where a confluence of veins creates a superficial venous plexus (Kiesselbach plexus)
Clinical Findings
It is important in all patients with epistaxis to consider underlying causes of the bleedingLaboratory assessment of bleeding parameters may be indicated, especially in recurrent cases
Once the acute episode has passed, careful examination of the nose and paranasal sinuses to rule out neoplasia and hereditary hemorrhagic telangiectasia is wise
Patients presenting with epistaxis often have higher blood pressures than control patients, but in many cases, blood pressure returns to normal following treatment of acute bleeding
Repeat evaluation for clinically significant hypertension and treatment should be performed following control of epistaxis and removal of any packing
Treatment
Most cases of anterior epistaxis may be successfully treated by direct pressure on the site by compression of the nares continuously for 15 minutesVenous pressure is reduced in the sitting position, and slight leaning forward lessens the swallowing of blood
Short-acting topical nasal decongestants (eg, phenylephrine, 0
125–1% solution, one or two sprays), which act as vasoconstrictors, may also help
When the bleeding does not readily subside, the nose should be examined, using good illumination and suction, in an attempt to locate the bleeding site
Topical 4% cocaine applied either as a spray or on a cotton strip serves both as an anesthetic and a vasoconstrictor
If cocaine is unavailable, a topical decongestant (eg, oxymetazoline) and a topical anesthetic (eg, tetracaine or lidocaine) provide similar results
When visible, the bleeding site may be cauterized with silver nitrate, diathermy, or electrocautery
A supplemental patch of Surgicel or Gelfoam may be helpful with a moisture barrier, such as petroleum-based ointment, to prevent drying and crusting
Warfarin may be continued in the setting of controlled epistaxis, although resorbable packing may preferable in these patients
Occasionally, a site of bleeding may be inaccessible to direct control, or attempts at direct control may be unsuccessful
In such cases, there are a number of alternatives
When the site of bleeding is anterior, a hemostatic sealant, pneumatic nasal tamponade, or anterior packing may suffice
There are a number of ways to do this, such as with several feet of lubricated iodoform packing systematically placed in the floor of the nose and then the vault of the nose, or with various manufactured products designed for nasal tamponade
About 5% of nasal bleeding originates in the posterior nasal cavity
Such bleeds are more commonly associated with atherosclerotic disease and hypertension
If an anteriorly placed pneumatic nasal tamponade is unsuccessful, it may be necessary to consult an otolaryngologist for a pack to occlude the choana before placing a pack anteriorly
In emergency settings, double balloon packs (Epistat) may facilitate rapid control of bleeding with little or no mucosal trauma
Because such packing is uncomfortable, bleeding may persist, and vasovagal syncope is quite possible, hospitalization for monitoring and stabilization is indicated
Opioid analgesics are needed to reduce the considerable discomfort and elevated blood pressure caused by a posterior pack
Surgical management of epistaxis, through ligation of the nasal arterial supply (internal maxillary artery and ethmoid arteries) is an alternative to posterior nasal packing
Endovascular embolization of the internal maxillary artery or facial artery is also quite effective and can allow very specific control of hemorrhage
Such alternatives are necessary when packing fails to control life-threatening hemorrhage
On very rare occasions, ligation of the external carotid artery may be necessary
After control of epistaxis, the patient is advised to avoid straining and vigorous exercise for several days
Nasal saline should be applied to the packing frequently to keep the packing moist
Avoidance of hot or spicy foods and tobacco is also advisable, since these may cause nasal vasodilation
Avoiding nasal trauma, including nose picking, is an obvious necessity
Lubrication with petroleum jelly or bacitracin ointment and increased home humidity may also be useful ancillary measures
Finally, antistaphylococcal antibiotics (eg, cephalexin, 500 mg orally four times daily, or clindamycin, 150 mg orally four times daily) are indicated to reduce the risk of toxic shock syndrome developing while the packing remains in place (at least 5 days)
When to Refer