chronic otitis media
chronic otitis media
ESSENTIALS OF DIAGNOSIS
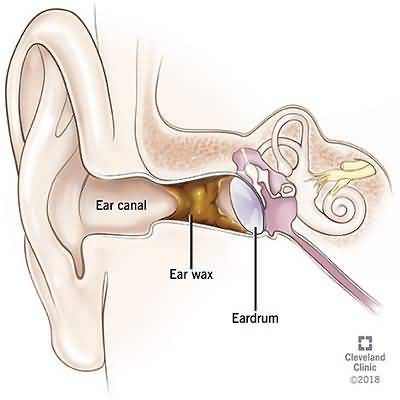
Acute otitis media with effusion of right ear, with multiple air-fluid levels visible through a translucent, slightly retracted, nonerythematous tympanic membrane
General Considerations
Chronic infection of the middle ear and mastoid generally develops as a consequence of recurrent acute otitis media, although it may follow other diseases and traumaPerforation of the tympanic membrane is usually present
The bacteriology of chronic otitis media differs from that of acute otitis media
Common organisms include P aeruginosa, Proteus species, Staphylococcus aureus, and mixed anaerobic infections
Clinical Findings
The clinical hallmark of chronic otitis media is purulent aural dischargeDrainage may be continuous or intermittent, with increased severity during upper respiratory tract infection or following water exposure
Pain is uncommon except during acute exacerbations
Conductive hearing loss results from destruction of the tympanic membrane or ossicular chain, or both
Treatment
The medical treatment of chronic otitis media includes regular removal of infected debris, use of earplugs to protect against water exposure, and topical antibiotic drops (ofloxacin 03% or ciprofloxacin with dexamethasone) for exacerbations
Oral ciprofloxacin, active against Pseudomonas, 500 mg twice a day for 1–6 weeks may help dry a chronically discharging ear
Definitive management is surgical in most cases
Successful reconstruction of the tympanic membrane may be achieved in about 90% of cases, often with elimination of infection and significant improvement in hearing
When the mastoid air cells are involved by irreversible infection, they should be exenterated at the same time through a mastoidectomy