External Otitis
External Otitis
ESSENTIALS OF DIAGNOSIS
General Considerations
External otitis presents with otalgia, frequently accompanied by pruritus and purulent dischargeThere is often a history of recent water exposure (ie, swimmer’s ear) or mechanical trauma (eg, scratching, cotton applicators)
External otitis is usually caused by gram-negative rods (eg, Pseudomonas, Proteus) or fungi (eg, Aspergillus), which grow in the presence of excessive moisture
In diabetic or immunocompromised patients, persistent external otitis may evolve into osteomyelitis of the skull base (so-called, malignant external otitis)
Usually caused by Pseudomonas aeruginosa, osteomyelitis begins in the floor of the ear canal and may extend into the middle fossa floor, the clivus, and even the contralateral skull base
Clinical Findings
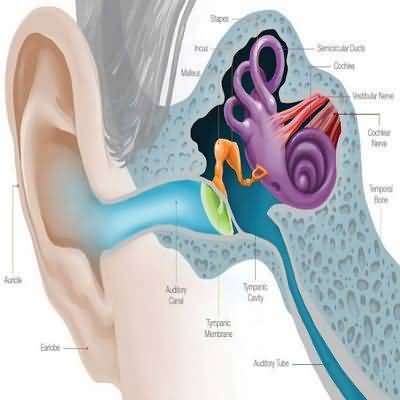
Examination reveals erythema and edema of the ear canal skin, often with a purulent exudate (Figure 8–1)Manipulation of the auricle elicits pain
Because the lateral surface of the tympanic membrane is ear canal skin, it is often erythematous
However, in contrast to acute otitis media, it moves normally with pneumatic otoscopy
When the canal skin is very edematous, it may be impossible to visualize the tympanic membrane
Malignant external otitis typically presents with persistent foul aural discharge, granulations in the ear canal, deep otalgia, and in advanced cases, progressive palsies of cranial nerves VI, VII, IX, X, XI, or XII
Diagnosis is confirmed by the demonstration of osseous erosion on CT scanning
Treatment
Treatment of external otitis involves protection of the ear from additional moisture and avoidance of further mechanical injury by scratchingIn cases of moisture in the ear (eg, swimmer’s ear), acidification with a drying agent (ie, a 50/50 mixture of isopropyl alcohol/white vinegar) is often helpful
When infected, an otic antibiotic solution or suspension of an aminoglycoside (eg, neomycin/polymyxin B) or fluoroquinolone (eg, ciprofloxacin), with or without a corticosteroid (eg, hydrocortisone), is usually effective
Purulent debris filling the ear canal should be gently removed to permit entry of the topical medication
Drops should be used abundantly (five or more drops three or four times a day) to penetrate the depths of the canal
When substantial edema of the canal wall prevents entry of drops into the ear canal, a wick is placed to facilitate their entry
In recalcitrant casesparticularly when cellulitis of the periauricular tissue has developed—oral fluoroquinolones (eg, ciprofloxacin, 500 mg twice daily for 1 week) are used because of their effectiveness against Pseudomonas
Any case of persistent otitis externa in an immunocompromised or diabetic indi- vidual must be referred for specialty evaluation
Treatment of “malignant external otitis” requires prolonged antipseudomonal antibiotic administration, often for several months
Although intravenous therapy is often required initially (eg, ciprofloxacin 200–400 mg every 12 hours), selected patients may be graduated to oral ciprofloxacin (500–1000 mg twice daily)
To avoid relapse, antibiotic therapy should be continued, even in the asymptomatic patient, until gallium scanning indicates marked reduction or resolution of the inflammation
Surgical debridement of infected bone is reserved for cases of deterioration despite medical therapy