Diabetic retinopathy is broadly classified as nonproliferative
Diabetic retinopathy is broadly classified as nonproliferative
Diabetic Retinopathy ESSENTIALS OF DIAGNOSIS
General Considerations
Diabetic retinopathy is broadly classified as nonproliferative, which is subclassified as mild, moderate, or severe, or proliferative, which is less common but causes more severe visual lossDiabetic retinopathy is present in about onethird of patients in whom diabetes has been diagnosed, and about one-third of those have sight-threatening disease
In the United States, it affects about 4 million people; it is the leading cause of new blindness among adults aged 20–65 years; and the number of affected individuals aged 65 years or older is increasing
Worldwide, there are approximately 93 million people with diabetic retinopathy, including 28 million with vision-threatening disease
Retinopathy increases in prevalence and severity with increasing duration and poorer control of diabetes
In type 1 diabetes, retinopathy is not detectable for at least 3 years after diagnosis
In type 2 diabetes, retinopathy is present in about 20% of patients at diagnosis and may be the presenting feature
Clinical Findings
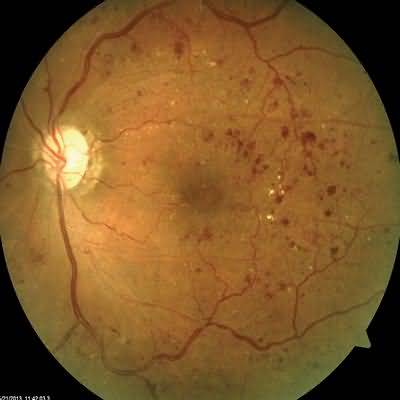
Clinical assessment comprises visual acuity testing, stereoscopic examination of the retina, retinal imaging with optical coherence tomography, and sometimes fluorescein angiographyNonproliferative retinopathy manifests as microaneurysms, retinal hemorrhages, venous beading, retinal edema, and hard exudates
Reduction of vision is most commonly due to diabetic macular edema, which may be focal or diffuse, but it can also be due to macular ischemia
Macular involvement is the most common cause of legal blindness in type 2 diabetes
Macular edema may be associated with treatment with thiazolidinediones (glitazones)
Proliferative retinopathy is characterized by neovascu- larization, arising from either the optic disk or the major vascular arcades
Vitreous hemorrhage is a common sequela
Proliferation into the vitreous of blood vessels, with their associated fibrous component, may lead to tractional retinal detachment
Adult and adolescent patients with diabetes mellitus should undergo regular screening by fundal photography, commonly with centralized screening that may involve computer detection software programs, or slit-lamp examination
More frequent monitoring is required in women during pregnancy and in those planning pregnancy
Patients with type 2 diabetes mellitus should be screened shortly after diagnosis
Treatment
Treatment includes optimizing blood glucose, blood pressure, kidney function, and serum lipids, although such measures are probably more important in preventing the development of retinopathy than in influencing its subsequent courseFenofibrate and renin-angiotensin system inhibitors are beneficial even in established retinopathy
Macular edema and exudates, but not ischemia, may respond to laser photocoagulation; to intravitreal administration of a VEGF inhibitor (ranibizumab [Lucentis], pegaptanib [Macugen], bevacizumab [Avastin], or aflibercept [VEGF Trap-Eye, Eylea]) or corticosteroid (triamcinolone, dexamethasone implant [Ozurdex], or fluocinolone implant [Retisert, Iluvien]); to vitrectomy; or to intravitreal injection of a serine protease (ocriplasmin [Jetrea]) to release vitreo-retinal traction
Proliferative retinopathy is usually treated by panretinal laser photocoagulation, preferably before vitreous hemorrhage or tractional detachment has occurred
Regression of neovascularization can also be achieved by intravitreal injection of a VEGF inhibitor
In patients with severe nonproliferative retinopathy, fluorescein angiography can help determine whether panretinal laser photocoagulation should be undertaken prophylactically by determining the extent of retinal ischemia
Vitrectomy is necessary for removal of persistent vitreous hemorrhage, to improve vision and allow panretinal laser photocoagulation for the underlying retinal neovascularization, for treatment of tractional retinal detachment involving the macula, and for management of rapidly progressive proliferative disease
Proliferative diabetic retinopathy, especially after successful laser treatment, is not a contraindication to treat- ment with thrombolytic agents, aspirin, or warfarin unless there has been recent intraocular hemorrhage
When to Referal