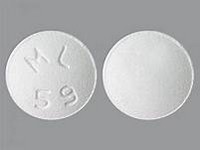
Fungizonel

Fungizone
CLINICAL USE
Antifungal agent: Systemic fungal infections (yeasts and yeast-like fungi including Candida albicans)DOSE IN NORMAL RENAL FUNCTION
250 micrograms – 1.5 mg/kg/day Can be given on alternate days if using a higher dosePHARMACOKINETICS
DOSE IN RENAL IMPAIRMENT
GFR (mL/MIN)
DOSE IN PATIENTS UNDERGOING RENAL REPLACEMENT THERAPIES
IMPORTANT DRUG INTERACTIONS
Potentially hazardous interactions with other drugs Ciclosporin: increased nephrotoxicity Tacrolimus: increased nephrotoxicity Increased risk of nephrotoxicity with aminoglycosides and other nephrotoxic agents and cytotoxics Cardiac glycosides: increased toxicity if hypokalaemia occurs Corticosteroids: increased risk of hypokalaemia – avoid concomitant use unless corticosteroids are required to control reactions Flucytosine: enhanced toxicity in combination with amphotericinADMINISTRATION
Reconstition
See SPC. Prepare intermittent infusion in glucose 5% (incompatible with sodium chloride 0.9%, electrolytes or other drugs). Reconstitute vial contents with water for injection. pH should be adjusted to >4.2 Dilute to a concentration of 10 mg in 100 mLRoute
IV infusion
Rate of Administration
2–6 hours If given over 12–24 hours there is a reduced incidence of side effectsComments
Minimum volume peripherally 0.2 mg/mL, centrally 0.5 mg/mL. (UK Critical Care Group, Minimum Infusion Volumes for fluid restricted critically ill patients, 3rd Edition, 2006) Higher rates of infusion are associated with greater risk of adverse reactions. Administration over less than 1 hour, particularly in renal failure, has been associated with hyperkalaemia and arrhythmias Paracetamol and parenteral pethidine may alleviate rigors associated with amphotericin administration. Can also give antihistamines and corticosteroids to control reactions Flush existing IV line with glucose 5% before and after infusion administration For patients on CAV/VVHD, amphotericin should be given into the venous return of the dialysis circuit Amphotericin iV – Fungizone t is not licensed for use by anyone else. AMPhoTEriCin iV – FUnGiZonE 51OTHER INFORMATION
*** AMPHOTERICIN IS HIGHLY NEPHROTOXIC *** Permanent renal impairment may occur, particularly in patients receiving conventional amphotericin B at doses >1 mg/kg/day, or with pre-existing renal impairment, prolonged therapy, sodium depletion or concurrent nephrotoxic drugs Nephrotoxicity may be reduced by giving anIV infusion
of sodium chloride 0.9% 250–500 mL over 30–45 minutes immediately before administering amphotericin B Can cause distal tubular acidosis May cause polyurea, hypovolaemia, hypokalaemia and acidosis. Amphotericin and flucytosine act synergistically when co-administered enabling lower doses to be used effectively A test dose of amphotericin is recommended at the beginning of a new course (1 mg over 20–30 minutes then stop and observe for 30 minutes) Monitor renal function, full blood count, potassium, magnesium and calcium levels Liposomal amphotericin is considerably less nephrotoxic compared with conventional amphotericin B, but is considerably more expensive There are reports of the use of amphotericin in 20% lipid solution being as well tolerated as liposomal amphotericin
See how to identify renal failure stages according to GFR calculation
See how to diagnose irreversible renal disease
Home