with branch being four times more common
The major predisposing factors are the etiologic factors associated with arteriosclerosis
Clinical Findings
Symptoms and Signs
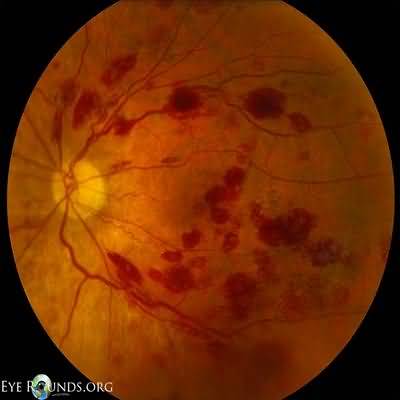
Ophthalmoscopic signs of central retinal vein occlusion include widespread retinal hemorrhages, retinal venous dilation and tortuosity, retinal cotton-wool spots, and optic disk swelling
Branch retinal vein occlusion may present in a variety of ways
Sudden loss of vision may occur at the time of occlusion if the fovea is involved or some time afterward from vitreous hemorrhage due to retinal new vessels
More gradual visual loss may occur with development of macular edema
In acute branch retinal vein occlusion, the retinal abnormalities (hemorrhages, venous dilation and tortuos- ity, and cotton-wool spots) are confined to the area drained by the obstructed vein
To assess possible reversible risk factors, check blood pressure and ask about tobacco smoking in all patients and ask women about estrogen therapy (including combined oral contraceptives)
Laboratory Findings Obtain screening laboratory studies for diabetes mellitus, hyperlipidemia, and hyperviscosity (especially in simultaneous bilateral disease), including serum protein electrophoresis for paraproteinemia
Particularly in younger patients, consider obtaining antiphospholipid antibodies, lupus anticoagulant, tests for inherited thrombophilia, and plasma homocysteine levels
Complications If central retinal vein occlusion is associated with widespread retinal ischemia, manifesting as poor visual acuity (20/200 [6/60] or worse), florid retinal abnormalities, and extensive areas of capillary closure on fluorescein angiogra- phy, there is a high risk of development of neovascular (rubeotic) glaucoma, typically within the first 3 months
Branch retinal vein occlusion may be complicated by peripheral retinal neovascularization or chronic macular edema
Treatment
Eyes at risk for neovascular glaucoma following ischemic central retinal vein occlusion can be treated by panretinal laser photocoagulation prophylactically or as soon as there is evidence of neovascularization, the latter approach necessitating frequent monitoring
Regression of iris neovascularization has been achieved with intravitreal injections of bevacizumab
In branch retinal vein occlusion complicated by retinal neovascularization, the ischemic retina should be laser photocoagulated
Intravitreal injection of ranibizumab (Lucentis), pegaptanib (Macugen), bevacizumab (Avastin), or aflibercept (VEGF Trap-Eye, Eylea), is beneficial in chronic macular edema due to either branch or nonischemic central retinal vein occlusion
Intravitreal triamcinolone improves vision in chronic macular edema due to nonischemic central retinal vein occlusion, whereas an intravitreal implant containing dexamethasone is beneficial in both central and branch retinal vein occlusion
Retinal laser photocoagulation may be indicated in chronic macular edema due to branch, but not central, retinal vein occlusion
Prognosis
In central retinal vein occlusion, severity of visual loss initially is a good guide to visual outcome
Initial visual acuity of 20/60 (6/18) or better indicates a good prognosis
Visual prognosis is poor for eyes with neovascular glaucoma
In branch retinal vein occlusion, visual outcome is determined by the severity of macular damage from hemorrhage, ischemia, or edema
When to Refer
All patients with retinal vein occlusion should be referred urgently to an ophthalmologist