Primary ocular herpes simplex virus infection may mani fest as lid, conjunctival, or corneal ulceration. The ability of the virus to colonize the trigeminal ganglion leads to recurrences that may be precipitated by fever, excessive exposure to sunlight, or immunodeficiency.
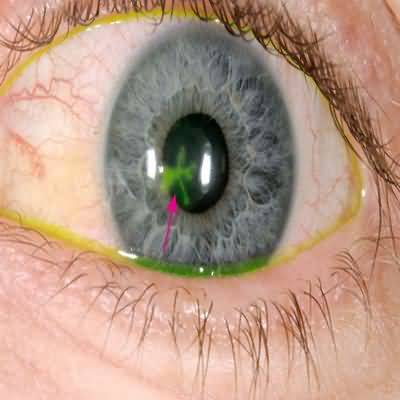
The dendritic (branching) corneal ulcer is the most characteristic manifestation of recurrent ocular disease.
More extensive (“geographic”) ulcers also occur, particularly if topical corticosteroids have been used.
The corneal ulcers are most easily seen after instillation of fluorescein and examination with a blue light. Such corneal epithelial disease in itself generally does not lead to corneal scarring.
It responds well to simple debridement and patching. More rapid healing can be achieved by the addition of topical antivirals, such as trifluridine drops, ganciclovir gel, or acyclovir ointment , or oral antivirals, such as acyclovir, 400–800 mg five times daily. Long-term oral acyclovir, 400 mg twice daily; famciclovir, 250 mg once daily; or valacyclovir, 500 mg once daily, reduces the rate of recurrent epithelial disease, particularly in atopic individuals.
Stromal herpes simplex keratitis produces increasingly severe corneal opacity with each recurrence.
Topical antivirals alone are insufficient to control stromal disease, so topical corticosteroids are used as well but they may enhance viral replication, exacerbating epithelial disease, and steroid dependence is common. Oral acyclovir, 200–400 mg five times a day, is often helpful in the treatment of severe herpetic keratitis. Severe stromal scarring may require corneal grafting, but the overall outcome is relatively poor.
Caution: For patients with known or possible herpetic disease, topical corticosteroids should be prescribed only with ophthalmologic supervision.
When to Refer
Any patient with a history of herpes simplex keratitis and an acute red eye should be referred urgently to an ophthalmologist.