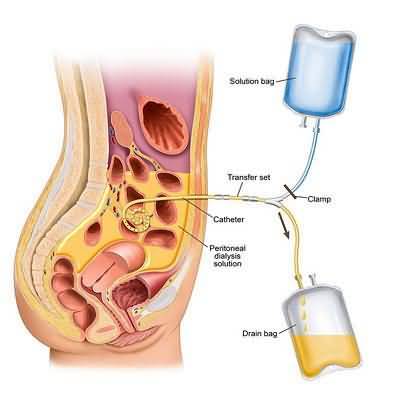
Peritoneal dialysis (PD) catheter insertion can be accomplished by any 1 of 3 techniques.
These include dissective or surgical, the blind or modified Seldinger, and laparoscopic techniques.
The dissective technique solely utilized by surgeons, places the catheter by mini laparotomy under general anesthesia. In the blind or modified Seldinger technique a needle is inserted into the abdomen, a guide-wire placed, a tract dilated and the catheter is inserted through a split-sheath, all without visualization of the peritoneal cavity. Of the various laparoscopes, peritoneoscopic insertion uses a small optical peritoneoscope for direct inspection of the peritoneal cavity and identification of a suitable site for the intraperitoneal portion of the catheter. Hence, of the 3 techniques, only the latter allows for the direct visualization of the intraperitoneal structures.
This technique can be easily used by nephrologists as well as surgeons.
Peritoneoscopic placement varies from traditional laparoscopic techniques by using: a much smaller scope (2.2 mm diameter) and puncture size, only one peritoneal puncture site, a device to advance the cuff into the musculature, air in the peritoneum rather than CO2, and local anesthesia rather than general anesthesia.
Prospective randomized and nonrandomized studies have shown that PD catheters peritoneoscopically placed by nephrologists have less incidence of complications (infection, exit site leak) and longer catheter survival rates than those inserted surgically.
The current review focuses on the peritoneoscopic insertion of PD catheter and presents some of the complicating issues (bowel perforation, catheter migration, and prior abdominal surgery) related to this procedure.