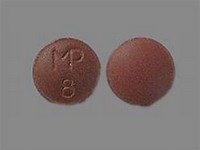
imipramine hydrochloride
CLINICAL USE
Tricyclic antidepressant
DOSE IN NORMAL RENAL FUNCTION
25 mg up to 3 times daily increasing up to 150–200 mg daily; maximum 300 mg in hospital patients
PHARMACOKINETICS
DOSE IN RENAL IMPAIRMENT
GFR (mL/MIN)
DOSE IN PATIENTS UNDERGOING RENAL REPLACEMENT THERAPIES
IMPORTANT DRUG INTERACTIONS
Potentially hazardous interactions with other drugs
ADMINISTRATION
Reconstition
–
Route
Oral
Rate of Administration
–
Comments
–
OTHER INFORMATION
Imipramine metabolised to active metabolite desipramine, which has <1% urinary excretion